By William Misner, Ph.D.
INTRODUCTION
Why should the body be exposed to a minimal repletion electrolyte dose during extreme losses? Hypothetically electrolyte absorption should occur under the body’s radar, without triggering a cascade of hormonal signals alter excretion rate by the kidneys. This hypothetically supports for taking the low sodium model as opposed to a higher sodium electrolyte. It needs to be emphasized that substrate repletion is never completed during high metabolic aerobic expense above sedentary state. Glycogen/glucose, electrolytes, fluids, and numerous other substrates are lost faster than they can be replaced during exercise. Waste matter and free radicals accumulate at 12-20 times that rate which is normally restored during sedentary inactivity. To suggest that a substrate must be replaced at or near the rate it is lost, is to suggest that 1-liter water, 2000 milligrams sodium, and 700 calories per hour must be consumed. We have observed that athletes who consume only 50% of this amount are more likely to have problems than those who consume 1/4 of the lost metabolites during ultra endurance exercise. This material may be shared in its entirety. This is a complex issue, since individual variations are difficult to explain without full understanding of how the individual response is effecting excretion versus re-absorption of sodium, fluids, and other substances. Reinking and Bennett have composed a texts to explain some of the complexities, though keep in mind neither suggests that one dose-size fits all.
There is a point in time at which the body cannot replace losses from exogenous sources. Overdose of a single electrolyte at its repletion rate may lead to other imbalances triggering other systemic reactions that may lead to further problems that may inhibit performance. This suggests adding small dose electrolyte dose before detectable overdose triggers hormone-activated mechanisms further impeding natural outcome and performance progress. Aldosterone levels control the rate of sodium recirculated in the human body.
ALDOSTERONE (Plasma) Males: 6-22 ng/dl is normal. Females: 4-31 ng/dl is normal. Pregnant females: 18 – 100 ng/dl is normal. Aldosterone is synthesized in the adrenal cortex. It stimulates the kidney tubule cells to increase their REABSORPTION OF SODIUM BACK INTO THE BLOOD. NORMAL SERUM OR PLASMA LEVELS OF ALDOSTERONE ARE DEPENDENT ON THE SODIUM INTAKE AND WHETHER THE PATIENT IS UPRIGHT OR SUPINE. High sodium intake will tend to suppress serum aldosterone, whereas low sodium intake will elevate serum aldosterone. The reference intervals for serum (plasma) aldosterone are based on normal sodium intake.
High Aldosterone levels occur in response to stress, renal dysfunction, adrenal cortical overactivity, pregnancy.
NORMAL ALDOSTERONE SERUM:
[A] Upright: 4.0-31.0 ng/dL
[B] Supine: <1.6-16.0 ng/dL
NORMAL ALDOSTERONE URINE:
NORMAL DIET: 6-25 µg/24 hrs
LOW SODIUM DIET: 17-44 µg/24 hrs
HIGH SODIUM DIET: 0-6 µg/24 hrs
NORMAL URINE VALUES OF ALDOSTERONE ARE DEPENDENT ON SODIUM INTAKE
Normal sodium intake: 100-200 mEq
Low sodium intake: < 25 mEq
High sodium intake: > 200 mEq
ELECTROLYTE REPLACEMENT: AN OVERVIEW
The thirst mechanism in animals is a complex interaction of control centers in the brain and hypothalamus; though the details of that mechanism go well beyond the scope of this note, it is important to know that the thirst mechanism is linked to water loss. When total body fluid volume decreases by 0.5-1.0%, the thirst mechanism asserts itself. Approximately 55% of water intake is derived directly from fluids, 35% from food, and 10% from water produced as a byproduct of metabolism. Kidneys excrete approximately 1 to 2 liters of urine per day. Approximately 900 milliliters (ml) of this amount is obligatory water excretion that gets rid of solutes and is constant from day to day. The remainder is excreted according to the fluctuating needs of the body and the changing renal tubular reabsorption rate. The process by which the body loses water through the skin is called insensible water loss. Approximately 350 ml of water is excreted by diffusion through the skin, while another 100 ml is lost through normal perspiration. Heavy perspiration in response to heat evaporative cooling need may cause a greater loss. Water loss through respiration is about 350 ml per day, varying with climate. About 150 to 200 ml is lost through feces. There are three main types of solutes: electrolytes, plasma proteins, and small organic compounds. Electrolytes are chemical elements such as acid, alkali, or salt dissociated into ions. SODIUM COMPRISES ABOUT 45% OF THE TOTAL ELECTROLYTE CONCENTRATION. The SODIUM CATION in extracellular fluids [ECF] is the primary osmotic force in maintaining maintains the necessary water volume for cells. Chloride, the main anion in ECF, provides balance to the SODIUM CATION. The intracellular fluids [ICF] contains POTASSIUM & PHOSPHATE. The concentration of electrolytes in a solution is based on the number of particles in solution. This concentration is measured in milliequivalents (mEq). On a broader, less localized level, the kidney is primarily responsible for maintaining water and electrolyte balance in the body. The kidney is alternately triggered to action by the hormones vasopressin and aldosterone.
VASOPRESSIN, also called antidiuretic hormone (ADH), is secreted by the pituitary gland and stimulates the reabsorption of water. ADH secretion can be stimulated by a loss of body water, whether it is an actual loss or the result of a shift of water from plasma to interstitial ECF spaces as occurs in congestive heart failure. ALDOSTERONE, secreted by the adrenal gland, acts PRIMARILY TO CONSERVE SODIUM, but in doing so has the affect of controlling water loss. The mechanism of action of aldosterone is referred to as the renin-angiotensin-aldosterone mechanism. Renin is an enzyme secreted by the renal cortex into the blood under the circumstances of decreased sodium intake, sodium loss, or decreased fluid volume. Renin interacts with a serum globulin from the liver to form angiotensin I and angiotensin II in the blood. Angiotensin II increases the force of the heart beat, constricts arterioles, and diminishes renal blood flow. This triggers the release of aldosterone. ALDOSTERONE CAUSES THE KIDNEYS TO RETAIN AND REABSORB SODIUM. This action, in turn, conserves water and results in loss of potassium.
HORMONE-ACTIVATED KIDNEY RESPONSE [1]
The kidneys are essential adjuncts to the cardiovascular system. These organs control erythrocyte production, direct the release of vasoactive hormones and regulate both the blood composition and volume. The concepts of renal function will be reviewed in this chapter in order to serve as a basis for better understanding of the Regulation of Arterial Blood Pressure. Perhaps the best way to appreciate the role of the kidneys is to consider their blood supply. THE KIDNEYS ARE PLACED IN A STRATEGIC POSITION IN THE CIRCULATION AND, AT REST, RECEIVE 20-25% OF THE CARDIAC OUTPUT. This is a huge amount of blood for a pair of organs that represent only about 1% of the body mass. It is important to consider that fluid processing, by the kidney, alters blood volume and an altered blood volume, in turn, alters cardiac filling. Combined, both human kidneys have about two million nephrons. There are two basic parts to the nephron, a glomerulus and a renal tubule. The glomerulus, a knot of capillaries, receives blood from the afferent arteriole. Blood leaves the glomerulus via the efferent arteriole, which then forms vessels that cover the renal tubule. The renal tubule is comprised of Bowman’s capsule, the proximal convoluted tubule, the loop of Henle and the distal convoluted tubule. Many nephrons feed into a collecting duct and, ultimately, many collecting ducts flow into the ureter.
RENAL PROCESSES
FILTRATION – As blood flows through the glomerulus, fluid is filtered into Bowman’s capsule. As we saw in the microcirulation lab, a number of osmotic and hydraulic forces influence this fluid movement. In humans, the GLOMERULAR FILTRATION RATE IS ABOUT 125 ML FLUID/MIN. This process is rather indiscriminate since everything except for the cells and large protein molecules filter from the glomerulus into Bowman’s capsule. In other words, many valuable components such as water, ions, amino acids, vitamins and glucose are lost from the blood during filtration. If all of the glomerular filtrate resulted in urine, an individual would excrete (and replace) 180 liters per day. OBVIOUSLY, FURTHER PROCESSING STEPS MUST RECOVER MOST OF THIS FILTRATE.
REABSORPTION
The proximal convoluted tubule is lined with cells that actively transports solutes from the lumen of the tubule back into the blood (remember that the tubule is cover with peritubular capillaries). This process is specifically referred to as tubular reabsorption. Water movement is linked to this active transport of solutes and results in reabsorption of most of the filtered water. Additional reabsorption of solutes also can occur in other portions of the renal tubule. Sodium is mostly reabsorped in the proximal tubule but a small portion is reabsorped in the loop of henle and in the distal tubule. The reabsorption of sodium in the distal tubule is significant because it is under the control of the adrenal hormone, ALDOSTERONE.
SECRETION
As the forming urine passes through the renal tubule, some solutes are moved, via active transport, from the blood to the lumen of the tubule. This process is called tubular secretion. In particular, substance such as creatinine, urea, organic acids and potassium are secreted. Potassium secretion in the distal convoluted tubule is of particular interest because it is linked to sodium reabsorption and, thus, is also under the control of ALDOSTERONE.
CONCENTRATION
As the forming urine reaches the end of the distal tubule, the osmotic concentration is about the same as that of the blood (˜300 mOsm/liter). If urine were excreted at this concentration, a person consuming a normal amount of fluid would become dehydrated due to a large water loss. In cases of normal hydration, urine must be concentrated before it leaves the kidney. They key to urine concentration is a solute gradient that is established in the tissues of the renal medulla. If we were to measure osmotic concentrations of tissue in the kidneys, we would find that the osmotic concentration in the cortex is about 300 mOsm/liter and progressively increases until it reaches 1,200 mOsm/liter in the innermost zone of the medulla. Passing through the medullary solute gradient are the loops of Henle, the vasa recta and the collecting ducts.
A NUMBER OF FACTORS CONTRIBUTE TO THE FORMATION OF THE MEDULLARY SOLUTE GRADIENT AND INCLUDE:
1) Sodium and chloride transport in the upper, thick portion of the loop of henle.
2) A countercurrent multiplier in the loop of henle.
3) Water impermeability of the distal tubule.
4) Urea moving from the collecting duct.
5) The unique, hair-pin shape of the vasa recta.
[The exact mechanism involved in forming this gradient is beyond the scope of this text.]
As fluid moves down the collecting duct, it encounters an increasingly greater osmotic gradient in the surrounding medullary tissue. Water, in response to the concentration gradient, tends to diffuse out of the collecting ducts into the surrounding tissue. As a result of this water extraction the urine in concentrated. Water, entering the medullary tissue, is then picked up by the vasa recta and returned to the circulation
VASOPRESSIN (ANTIDIURETIC HORMONE, ADH) CONTROLS WATER/FLUID LEVELS
ADH REGULATES WATER EXTRACTION FROM THE COLLECTING DUCT. WHEN INCREASED BLOOD OSMOTIC CONCENTRATION is sensed in the osmotic center of the brain, ADH is released by the posterior pituitary (neurohypophysis). This hormone travels through the blood, binds to receptors on the collecting ducts and CAUSES INCREASED WATER PERMEABILITY. As a result, more water is extracted and the urine becomes more concentrated. IN CASES OF OVER-HYDRATION, ADH is no longer released, the collecting duct becomes less permeable to water and more water is lost to the urine. ADH is also called VASOPRESSIN because this molecule promotes increased blood pressure via vasoconstriction (i.e., a VASOPRESSOR ACTION).
RENIN-ANGIOTENSIN-ALDOSTERONE SYSTEM (RAAS)
This regulatory system, based in the kidneys, plays a key role in REGULATING BLOOD SODIUM CONCENTRATION, BLOOD POTASSIUM CONCENTRATION, BLOOD VOLUME AND BLOOD PRESSURE. The juxtaglomerular apparatus involves a portion of the distal tubule that has folded back toward the glomerulus (called the macula densa) plus a section of cells lining the afferent arteriole (the juxtaglomerular cells). The juxtaglomerular apparatus is able detect changes in sodium levels and renal blood pressure and flow. If sodium levels drop or if pressure or flow in the afferent arteriole drops, RENIN, a molecule stored in the juxtaglomerular cells in a precursor form, is released into the circulation. In the blood, RENIN converts circulating angiotensinogen into a decapeptide, angiotensin I. As ANGIOTENSIN I passes through the lungs it is converted into ANGIOTENSIN II (an octapeptide) by angiotensin converting enzyme (ACE) contained within the endothelial cells of the pulmonary vessels (minor conversion also occurs in other organs). Angiotensin II is a powerful vasoconstrictor and will cause an increase in blood pressure. Note that this action counters the original stimulus of decreased renal blood pressure. Angiotensin II also stimulates thirst via the central nervous system and stimulates ADH RELEASE. THESE ACTIONS WILL EVENTUALLY INCREASE BLOOD VOLUME. ADH CAUSES VASOCONSTRICTION. A final action of angiotensin II is to stimulate ALDOSTERONE production and release from the adrenal cortex. ALDOSTERONE IS A STEROID HORMONE THAT PROMOTES SODIUM REABSORPTION IN THE DISTAL TUBULE. INCREASED SODIUM REABSORPTION COUNTERS THE OTHER STIMULUS THAT TRIGGERS RENIN RELEASE. INCREASED SODIUM REABSORPTION WILL BE ACCOMPANIED WATER RETENTION AND INCREASED BLOOD VOLUME. [Angiotensin II formation: a decrease in serum sodium (or increase in serum potassium) triggers a chain of events that ultimately results in the secretion (and possible synthesis) of aldosterone by the adrenal cortex culminating in an action of this mineralocorticoid on the renal tubules to increase sodium reabsorption.]
CONTROL OF SERUM POTASSIUM
The renin-angiotensin-aldosterone system also plays a crucial role in regulating plasma potassium levels. Hyperkalemia, increased serum potassium, causes cardiac paralysis. INCREASE IN SERUM POTASSIUM DIRECTLY STIMULATES THE ADRENAL CORTEX TO PRODUCE AND RELEASE ALDOSTERONE. The increased sodium reabsorption in the distal tubule, caused by ALDOSTERONE, is linked to potassium secretion; the end result will be a reduced serum potassium concentration.
RELATION OF THE RENIN-ANGIOTENSIN-ALDOSTERONE SYSTEM (RAAS) TO OTHER VASOACTIVE SUBSTANCES
The renin-angiotensin-aldosterone system is closely linked to a clotting factor, plasmin and the kallikrein-kinin system. Kinins are vasodilators that are formed from tissue substrates called kininogens. This conversion is promoted by the action of KALLIKREINS, a class of proteolytic enzymes.
DIURETICS
DIURETIC THERAPY is commonly used to treat cardiovascular disorders such as congestive heart failure. The actions of some types of diuretics are listed below. Water, alcohol, caffeine and acidifying salts are typically not used in clinical situations. Keep in mind that when a solute is excreted water will follow.
The following table summarizes the actions of common diuretics:
| DIURETIC AGENT >>> | MECHANISM OF ACTION |
| Water >>> | Inhibits ADH release |
| Ethanol >>> | Inhibits ADH release |
| Caffeine >>> | Constricts efferent arteriole, glomer-filtration |
| (CaCl2, NH4 Carbonic anhydrase inhibitors >>> | H+ buffered, Na+ excreted with excess anions |
| Carbonic anhydrase inhibitors | Decrease H+ excretion, results in increased Na+ and K+ excretion |
| Loop diuretics such as furosemide (Lasix) and ethacrynic acid (Edecrin) >>> | Inhibit Na+/Cl- reabsorption in loop of Henle |
| Potassium sparing, sodium diuretics >>> | Decreases Na+/K+ exchange pump in distal tubule by inhibiting aldosterone |
NORMAL PHYSIOLOGY
L-Arginine VASOPRESSIN (AVP, ADH), a nonapeptide, is synthesized in the bodies of magnocellular neurons in the paired supraoptic nuclei and paraventricular (lateral to the 3rd ventricle) nuclei and transported down axons which form the pituitary stalk in granules bound to neurophysin & glycoprotein to be stored in the posterior pituitary axon terminals. STORES ARE SUFFICIENT FOR 5-10 DAYS OF MAXIMUM ANTIDIURESIS OR ONE MONTH OF NORMAL ANTIDIURESIS. AVP is released in free form (does not bind to neurophysin at blood pH), and is degraded in the brain, liver, and kidney. AVP IS ALSO TRANSPORTED DIRECTLY TO THE ANTERIOR PITUITARY, WHERE IS STIMULATES ACTH SECRETION. AVP has antidiuretic activity by binding V2 receptors in kidney, stimulating cAMP production by adenyl cyclase, which leads to synthesis & insertion of aquaporin-2 water channels in cells of the collecting tubules, allowing water reabsorption in the hypertonic medulla. Water exits basolaterally via constitutively expressed aquaporins 3 and 4. ABSENCE OF AVP LEADS TO EXCRETION OF LARGE VOLUMES OF DILUTE URINE. Other effects of AVP: acts at a pressor agent at supraphysiologic levels (as in severe hypovolemia) by binding V1a receptors on blood vessels, which increase intracellular calcium and cause smooth muscle contraction. V1a receptors are found on vascular smooth muscle, liver, brain, renal medulla, testes, and platelets. AVP stimulates hepatic glycogenolysis via the V1a receptor. A new V3 (V1b) receptor has been cloned; like the V1a receptor, it acts via phospholipase C. It is found in the anterior pituitary, kidney, and in corticotropic pituitary tumors.
REGULATION OF AVP RELEASE: Integration of AVP secretion and thirst maintains plasma osmolality tightly at 280-290 mOsm/kg. PLASMA OSMOLALITY [Posm]: Anterior hypothalamic osmoreceptors (anterior to the 3rd ventricle) are very sensitive to changes in Posm (respond to change as low as 1%), and suppress AVP release when Posm < 280 mOsm/kg. Posm values less than those necessary to turn off AVP will not result in any increase in water excretion (18-20 L/d maximum), unless intake is extreme. As Posm increases, there is a linear increase in [AVP]. WHEN POSM EXCEEDS 292-5 mOsm/kg, plasma AVP reaches levels (~ 6 pg/mL) sufficient for maximum antidiuresis (Uosm > 800 mOsm/kg, Uvol < 2 L/d), with no further decrease in urine volume with higher Posm. THIRST IS STIMULATED AT—–>290 mOsm/kg.
PLASMA VOLUME: Baroreceptors (stimulated by hypervolemia, inhibited by hypovolemia) inhibit AVP release via cranial nerves IX, X. The atrial cardiopulmonary low-pressure baroreceptors are less sensitive than osmoreceptors, requiring a 5-10% decrease in blood volume before AVP is released. Severe hypovolemia, however, triggers the sino-aortic high-pressure baroreceptors to cause exponential increases in AVP, which may be high enough to exert a pressor effect. Interaction of osmo- and baroreceptors: A decrease in left atrial pressure (as in hypovolemia, hypotension) leads to a reduction of the osmotic threshold and increases the sensitivity for osmotic AVP release. Volume expansion dampens the sensitivity for osmotic AVP release. Nausea is a very potent and rapid stimulus for AVP release, even up to 100-1000 times basal level. May be responsible for increases in AVP seen with chemotherapy, DKA, vasovagal reactions, motion sickness, and hypoxia. Pain and emotional stress may also stimulate AVP release, as can IV metoclopramide. Hypoglycemia may also stimulate AVP release, which then stimulates glycogenolysis.
THIRST REGULATION: osmoreceptors located nearby (not the same) initiate thirst at a higher Posm than the threshold for AVP release. Hypovolemia also triggers thirst even if Posm is normal [2].
ELECTROLYTE BALANCE
SODIUM<< >>POTASSIUM<< >>MAGNESIUM<< >>CALCIUM [3]
I. SODIUM NA+ ELECTROLYTE WATER BALANCE AND NEUROMUSCULAR MEMBRANE EXCITABILITY
-Major Cation in the extracellular fluids [ECF]- Water balance and neuromuscular membrane excitability
-Most Sodium is in the extracellular fluids [ECF], while intracellular levels of Sodium are relatively low.
-Sodium regulation at the cellular level is controlled by the Sodium-Potassium pump
-Body levels of Sodium (Sodium retention/excretion) are controlled by aldosterone.
-Aldosterone is controlled by the renin-angiotension system
HYPONATREMIA- LOW SODIUM – CAUSES OF ALTERATIONS IN SODIUM LEVELS
-Loss of Sodium from fluid loss
-Diuretics-Vomiting, Sweating, Bleeding, SIADH, Renal Failure -(inability to concentrate and save sodium)
-Movement of Sodium out of the ECF
-Failure of the Sodium Potassium Pump, Diabetic Ketoacidosis, Hypoxia, Liver Failure (Third Spacing)
-Dilution of Sodium from fluid overload
-Fresh water Drowning
-Over administration of Hypotonic Fluids
HYPONATREMIA – LOW SODIUM SIGNS AND SYMPTOMS OF ALTERATIONS IN SODIUM:
-Confusion
-Headache
-Nausea and Vomiting
-Generalized Muscle Weakness progressing to coma -Late
TREATMENT OF LOW SODIUM LEVELS
Monitor I&O, Wt, V/S, LOC, Serum Sodium and Serum Osmolarity -expect H/A
Restrict hypotonic fluids as ordered
Encourage foods or fluids high in Sodium
Careful use of Hypertonic IV fluids
CAUSES OF ALTERATIONS IN SODIUM LEVELS: HYPERNATREMIA – HIGH SODIUM
-Renal Failure (inability to excrete Sodium)
-Hypertonic IV fluids and/or tube feedings
-Excessive Salt Ingestion
-Decreased Fluid Intake
-Diabetes Insipidus (Not Enough ADH)
-Aldosteronism – leads to Sodium and Water Retention
HYPERNATREMIA- HIGH SODIUM SIGNS AND SYMPTOMS
-Hyper Reflexes
-Hypertension
-Seizures
TREATMENT OF HIGH SODIUM LEVELS
Monitor I&O, Wt, V/S, LOC, Serum Sodium and Serum Osmolarity -expect muscle twitching
Careful use of hypotonic or isotonic IV Fluids
Restrict Food, Fluids and Meds high in Sodium.
Seizure Precautions
———————————————————
II. POTASSIUM (K+) 3.5-5.5 mEq/L
-Critical for electrical conduction of nerve impulses-particularly cardiac electrical conduction
-Potassium is the major cation in the ICF
-Potassium balance at the cellular level is maintained by the sodium-potassium pump.
-Body Potassium levels are maintained by the kidneys ability to retain extra Potassium if needed.
-Kidneys can excrete Potassium and in exchange for Sodium – controlled by aldosterone.
-The body is much more sensitive to small changes in Serum Potassium levels than to small changes in other Serum Electrolytes
HYPOKALEMIA, LOW POTASSIUM LEVELS CAUSES OF ALTERATIONS IN POTASSIUM LEVELS –
-Loss of K+ – excessive vomiting, suctioning, diarrhea
-Medications – Diuretics, Laxatives and Insulin
-Alkalosis
-Hemodilution from Over hydration, Renal tubular acidosis, Hepatic disease, hyperaldosteronism, Cushing’s Syndrome or tumors of the adrenal cortex
-Acute Alcoholism
HYPOKALEMIA SIGNS- LOW POTASSIUM
-Weakness, N/V, Constipation, and Motility-ileus
-Hypotension and elevated pulse due to decreased cardiac output
-Alkalosis
-Signs of Hyperkalemia – High Potassium
-Diarrhea
-LOC Changes -Apathy and Confusion
-Numbness in hands and feet
-Acidosis
-Bradycardia and Cardiac Arrhythmias leading to Cardiac Arrest
HYPOKALEMIA TREATMENT- LOW POTASSIUM
-Place patient on a cardiac monitor
-Prevent injury from decreased B/P and muscle weakness
-Watch for digitalis toxicity (in persons on digitalis).
-Be sure patient has urine output of at least 30 cc/hour before giving any K+ supplement
-Give oral K+ supplements with food.
***NEVER GIVE POTASSIUM IV PUSH -It must be diluted and given as a drip. Watch for signs of infiltration, K+ can cause necrosis of tissues.
-Teach client to increase K+ in diet to prevent recurrence
HYPERKALEMIA – HIGH POTASSIUM LEVELS CAUSES OF ALTERATIONS IN POTASSIUM LEVELS –
-Use of Salt substitutes or K+ supplements
-Receiving old or improperly administered blood
-Movement of K+ out of cells due to decreased functioning of Sodium Potassium Pump related to hypoxia and/or acidosis
-Cell destruction – crushing injuries, burns and hemolysis
-Inadequate Potassium Excretion – from decreased aldosterone related to Adrenalectomy or -Addison’s disease
TREATMENT OF ALTERATIONS IN POTASSIUM LEVELS
-Treatment of Hyperkalemia – High Potassium
-False high serum potassium levels can result from improper blood drawing techniques
-Place patient on a cardiac monitor
-Prevent injury from bradycardia and diarrhea
METHODS TO LOWER SERUM POTASSIUM:
-Kayexalate exchange resin – most effective as a retention enema but can be given orally.
-Calcium gluconate -slow IV drip
-Concentrated glucose and insulin mixture IV (helps move K+ into cells)
-Sodium Bicarb for acidosis
-Teach client to avoid foods high in K+, such as cantaloupe, bananas, apricots, broccoli, and salt substitutes
III. CALCIUM (Ca++) 4.0-5.5 mEq/L or 8.5-10.5 mg/dl
-Required for normal skeletal muscle, smooth muscle, and cardiac muscle contraction. Also needed for blood clotting.
-Calcium is taken in through the diet, but Vitamin D must be present for it to be absorbed
REGULATION OF CALCIUM
-Varying rates of GI absorption – by Parathyroid control of Vitamin D absorption
-Parathyroid hormone – triggers calcium release from the bone and/or inhibits renal excretion of calcium
-Calcitonin – from the thyroid gland- causes ECF levels of calcium to decrease by inhibition of bone resorption (release) of calcium, inhibits Vitamin D absorption, and increases renal excretion of calcium
HYPOCALCEMIA – SERUM CALCIUM BELOW 4.5 mEq/L
-Usually due to a failure of normal regulatory mechanisms, such as acute or chronic renal failure
-Can also occur with: Malabsorption syndromes, Acute pancreatitis, and Alkalosis
HYPOCALCEMIA – PATHOPHYSIOLOGY
Calcium functions as a membrane stabilizer, so low levels increase excitability of nerves and muscles (especially GI). Although calcium is needed for blood clotting, prolonged deficiency or very low levels are needed before clotting mechanisms are altered Bones store calcium. If serum levels are low, bones release calcium and become osteoporotic Early ambulation and weight-bearing exercise can help prevent hypocalcemia.
HYPOCALCEMIA SIGNS AND SYMPTOMS
-Muscle spasms, cramps, and tremors
-Hyperactive reflexes
-Diarrhea
-Tingling of the fingers, toes, lips and face
-TETANY
-Positive Trousseau’s sign – Carpopedal Spasm (hand spasm when B/P cuff inflated 3-4 minutes).
-Positive Chvostek’s sign (tap facial nerve)
-Seizures
-Arrhythmia
-EKG Changes
TREATMENT OF HYPOCALCEMIA
-Monitor lab for other disturbances such as hypokalemia, hyperphospatemia, hypomagnesemia, and alkalosis
-Cardiac Monitor
-Seizure precautions
-Private room to decrease external stimuli
-Administer Oral calcium supplements and/or Vitamin D for mild to moderate hypocalcemia.
-Give oral calcium between meals to increase intestinal absorption.
-Administer IV Calcium for severe hypocalcemia via slow IV bolus followed by slow IV drip
-Watch for infiltration, calcium can cause necrosis and tissue sloughing.
-NEVER GIVE CALCIUM IM. Check Chvosteck’s sign every hour when giving IV calcium.
-Teach Patient about foods and fluids high in Calcium
HYPERCALCEMIA – SERUM CALCIUM ABOVE 5.5 MEQ/L ETIOLOGY
-Disturbances in regulatory functioning which can cause hypercalcemia
-Decreased renal excretion
-Diuretic use that enhance calcium reabsorption
-Too much parathyroid hormone
-Hyperthyroidism
-Cancer
-Abnormal parathyroid hormone production
-Excessive Intake of Calcium
HYPERCALCEMIA SIGNS
-Related to decreased excitability of nerves and muscles and increased blood clotting.
-Muscle weakness
-Nausea, vomiting, constipation
-Check for hypoactive bowel sounds
-Extreme Thirst
-Polyuria (if normal kidney function)
-Kidney Stones
-Blood clots
-Check for Homan’s Sign
-Arrhythmias
-EKG changes
TREATMENT OF HYPERCALCEMIA [Dialysis may be used in severe cases ]
-Monitor High Risk Patients: those on long term bed rest, with cancer, with hyperparathyroidism
-Increase fluid intake to 3-4 liters daily
-If low serum Phosphorus, administer phosphorus orally, rectally, or IV
-Corticosteroids can decrease GI absorption of Calcium
-Moderate to Severe Hypercalcemia, give IV N/S at 200 ml/hr to flush Calcium from system
-Administer loop diuretics to prevent volume overload with N/S
-IV calcitonin will temporarily lower serum Ca levels
V. MAGNESIUM (MG ++) 1.5-2.5 MEQ/L
-Needed to prevent overexcitability of muscles
-Mg has a sedative effect on the neuromuscular junction, inhibits acetylcholine release, and diminishes muscle cell excitability
-Acts as a co- factor in enzyme reactions
MG IS NEEDED for Muscle contraction, Nerve conduction, Blood clotting, Carbohydrate metabolism, ATP activation, B vitamin activation, DNA, and Protein synthesis.
HYPOMAGNESEMIA – SERUM LEVELS BELOW 1.5 MEQ/L
-Decreased GI absorption of Magnesium
-Malnutrition, TPN without Magnesium, prolonged N/G suctioning, vomiting, prolonged laxative abuse, diarrhea, destruction of the intestinal villi, alcoholism, cancer chemotherapy, excessive intake of Calcium or Vitamin D, High dose steroids
-Increased excretion of magnesium
diuretics, hypoparathyroidism, hypoaldosteronism, Pregnancy induced hypertension
-Movement of Mg from the ECF to the ICF
-Burns and debridement therapy, diabetic ketoacidosis, hypercalcemia
SIGNS AND SYMPTOMS OF HYPOMAGNESEMIA
-Tachycardia, cardiac arrhythmias and hypotension
-Painful paresthesia and muscle spasms
-Tetany, Hyperactive Reflexes
-Positive Chvostek’s and Trousseau’s
-LOC changes – confusion, agitation
-SEIZURES
HYPOMAGNESEMIA TREATMENT
-Monitor those on digitalis for toxicity (low Mg enhances digitalis actions)
-Cardiac Monitor and Seizure Precautions
-Treat low Mg with oral, IM or IV Mg Salts
–GIVE SLOWLY – IV Mg Acts immediately, can cause cardiac and/or respiratory arrest. For Seizures, give IV 10% MgCl no faster than 1.5 ml/min
-Watch Serum Calcium while giving Mg IV, as it will cause serum calcium levels to fall, be prepared to give calcium gluconate if needed.
-Urine output must be at least 30cc/hr for adequate Mg elimination
-Assess deep tendon reflexes during Mg treatment and hold Mg treatment if reflexes are absent
-Teach patient to increase foods high in Mg – Green Vegetables.
HYPERMAGNESEMIA – SERUM LEVELS ABOVE 2.5 MEQ/L
-Relatively Rare
-Usually caused by a combination of increased intake and decreased renal function
-Increased Intake antacids & laxatives
-IV administration of Mg
-Decreased Excretion
-renal insufficiency
-Addison’s disease
-Adrenalectomy
Hypermagnesemia Signs and Symptoms: [related to Mg sedative effect on the neuromuscular junction] is lethargy and drowsiness, Depressed respirations, Low B/P, Bradycardia progressing to cardiac arrest, Hypoactive reflexes, and Coma.
TREATMENT OF HYPERMAGNESEMIA
-Monitor those at risk
-On Mg supplements
-Renal failure
-Monitor V/S frequently, can decrease rapidly.
-Beware of Mg medications in persons with renal problems
-Be prepared to give calcium gluconate IV to temporarily relieve symptoms in an emergency.
-Teach the patient to avoid foods and medications high in Mg
WHAT IS THE ROLE OF ELECTROLYTES-FLUID-FUELS BALANCE IN HYPERTHERMIC [HOT] EVENTS?
For each kilogram of body mass a litre of fluid is lost. An athlete may account for the mass of fluid consumed during exercise versus total sweat rate, against their success in replacing fluid during the session. As muscle glycogen stores are rapidly metabolized nearly 2 full liters of water are released as byproducts of prolonged exercise. While it may be lost at nearly 34 fluid ounces per hour it can be replaced at only 16-24 fluid ounces per hour. Fluids lost in sweat may only be completely replaced during a time-aided reduced-rate-of-sweating recovery period. Cool drinks (ideally at 45-60 degrees F) are most rapidly absorbed in large volumes.
CARBOHYDRATES
A CARBOHYDRATE-ENHANCED FLUID DRINK MIX improves performance during moderate-high intensity exercise of longer than 90 minutes. A carbohydrate intake of 60-70 grams or 240-280 calories per hour will provide additional fuel when muscle carbohydrate stores become depleted postponing fatigue. This goal may be achieved by ingesting 600-720 mL/hr of drinks containing 12-15% (g/100mL) carbohydrate in long-chain malto-dextrins. Drinks within this range of concentration can deliver fluid and carbohydrate at a rate that will benefit performance.
ELECTROLYTES
SODIUM 0.3-0.6 g/l or 12-24 mmol/L or 3-6 ENDUROLYTES per 24-34 fluid ounces consumed each hour during exercise. Sodium promotes retention of the fluid consumed and prevents hyponatremia [diluted low serum sodium] in susceptible individuals. Carbohydrate-electrolyte drinks address the goals of post-exercise rehydration and recovery by promoting fluid intake, providing a source of carbohydrate for glycogen storage, and promoting fluid retention. The replacement of electrolyte losses, particularly sodium, plays an important role in maximizing post-exercise fluid retention. Although sodium replacement will occur in the diet over time, immediate replacement is important when the athlete needs to rehydrate quickly from a significant fluid deficit greater than -2% of fluid body mass loss.
POST EXERCISE DEHYDRATION
ORAL REHYDRATION solutions used in the clinical treatment of dehydration contain a higher concentration of sodium 50-90 mmol/L. Athletes may replace salt losses using a combination of sodium-containing drinks and the sodium found in post-exercise recovery meals and snacks, either as a component of the food or added to the meal [4, 5].
RESEARCH REVIEW OF ELECTROLYTE DEPLETION
Not a lot has changed except to note the human body adapts quite variably to demand and expenditure within time if it is stressed and replenished periodically. Each of us needs to duplicate racing in the conditions in our chosen events at least 6 weeks prior to the event up to 60% of the distance or up to 24 hours duration for a multi-day. As you will note below, the differences you may effect in your performance is dramatic from an electrolyte and muscle glycogen metabolic storage point of view. I have taken the liberty to post some of the research below, should you want to know these details from observed research on ultrarunners and triathletes. Research has shown that potentially fatal hyponatremia or dehydration may develop during prolonged extreme exercise in ultramarathon running or triathlons attempted in hot and/or humid weather conditions.
HYPONATREMIA [Low Sodium or water intoxication]
To determine the incidence of hyponatremia in athletes competing in ultradistance events, Noakes [6] “Measured serum sodium levels in 315 of 626 (50%) runners who were treated for collapse after two 90 km ultramarathon footraces (total starters 20,335; total finishers 18,031) and in 101 of 147 (69%) finishers in a 186 km ultratriathlon. In both races the athletes drank fluids with low sodium chloride content (less than 6.8 mmol.l-1). Hyponatremia (serum sodium level less than 130 mmol.l-1) was identified in 27 of 315 (9%) collapsed runners in the 90 km races and in none of the triathletes. In response to diuretic therapy, the runner with the most severe hyponatremia (serum sodium level = 112 mmol.l-1) excreted in excess of 7.5 l dilute urine during the first 17 h of hospitalization. These data suggest that, although symptomatic hyponatremia occurs in less than 0.3% of competitors during prolonged exercise even when they ingest little sodium chloride, it is found in a significant proportion (9%) of collapsed runners. A regulated contraction of the extracellular fluid volume would explain why the majority of athletes maintain normal serum sodium levels even though they develop a significant sodium chloride deficit during prolonged exercise. Alternatively, sodium chloride losses during prolonged exercise may be substantially less than are currently believed. Physicians treating collapsed ultradistance athletes need to be aware that as many as 10% or more of such patients may be hyponatremic.” Noakes [7] suggests water intoxication of hypotonic fluids [low electrolyte content] of 1000 ml./hour is likely to result in dilutional hyponatremia. He implied that athletes might do better on 500 ml/hour fluid intake as a correction device for ultra events performed in hyperthermic conditions. [500 ml=’s 16 ounces]
Review of the depleted differences between sodium [NA], chloride [CL], potassium [K] and Magnesium [MG] losses were measured* in the sweat of fit-acclimatized and unfit-unacclimatized athletes.
| ELECTROLYTE* | FIT & ACCLIMATIZED [grams/hour] | UNFIT & UNACCLIMATIZED[grams/hour] |
| SODIUM [NA] | 1.8 g | 3.5 g |
| CHLORIDE [CL] | 0.9 g | 1.4 g |
| POTASSIUM [K] | 0.2 g | 0.1 g |
| MAGNESIUM [MG] | 0.1 g | 0.1 g |
From: Verde, T, Shephard, RJ, Corey P, Moore R., Sweat Composition in Exercise and Heat, Journal of applied Physiology, 1982;53;6:1541-1543. This is overwhelming evidence in favor of fitness and acclimatization protocols progressively pursued during preparatory training.
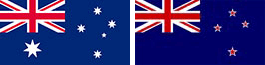
Speedy [9] described weight changes and the incidence of hyponatremia during an ultradistance triathlon in the athletes who attend medical care after the race. They researched the 1996 New Zealand Ironman Triathlon in which each athlete swam 3.8 km, cycled 180 km, and ran 42 km. Ninety-five athletes were seen for medical care after the race. One hundred sixty-nine athletes who did not attend for medical care were also weighed before and after the race. “Weights were measured at race registration and on finishing the race. Whole-blood sodium concentration was measured in those athletes with clinical evidence of fluid or electrolyte disturbances. Weights were significantly decreased at the end of the race in the athletes seeking medical care (n = 48, mean % delta wt = -2.5%, p < 0.001) and also in the athletes who did not seek medical care (n = 169, mean % delta wt = -2.9%, p < 0.001). Seventeen percent [17%] of race starters sought medical attention. Dehydration accounted for 26% of primary diagnoses and hyponatremia for 9%. One athlete with hyponatremia (Na 130 mEq/L) is described who drank 16 L over the course of the race, with a weight gain of 2.5 kg. [5.5 lbs.] This is consistent with the hypothesis of fluid overload as the cause of his hyponatremia. Hyponatremia accounted for four of five admissions to the hospital after the race. An inverse relationship between postrace sodium concentrations and percentage change in body weight was observed (r = -0.63).” Hyponatremia is an important risk to the health of athletes competing in an ultradistance triathlon, with fluid overload the likely cause. Other causes have been discussed for heat stress-induced performance retro-gradation by Toole [10]: “Thirty competitors in the Hawaii Ironman Triathlon were prospectively studied to determine whether fluid and electrolyte disturbances were causes for seeking race-day medical care. Athlete weights were significantly (p < 0.0001) decreased during the race, but decreases were not different in treated (n = 11; % delta wt -2.3 +/- 2.9) versus not treated (n = 19; % delta wt – 2.0 +/- 1.9) athletes. Hyponatremia occurred in nine athletes (30%), and hypomagnesemia in six (20%), but only half of athletes were either electrolyte imbalance sought care. Although athletes receiving medical care may have fluid and electrolyte problems, these abnormalities may also occur in healthy athletes.”
MEDICAL CORRECTION DISCUSSION
Cluitmans and Meinders [11] present concerns with a medical correction protocol: “Case reports and the literature on the treatment of severe hyponatremia were reviewed. It appeared that the conflicting opinions with respect to the rate of correction of severe hyponatremia could be reduced to not differentiating between acute and chronic hyponatremia, to using different criteria for this distinction, and to differences in treatment strategy. After reviewing the available data in the literature, it is suggested that hyponatremia should be classified as acute whenever the rate of decrease of serum sodium exceeds 0.5 mmol/L/hour. If it is unknown at which rate the hyponatremia has developed, it can be assumed to be acute if within a short period of time (two to three days), large quantities of fluid are ingested orally or administered parenterally, especially hypotonic fluids in the presence of impaired water excretion. In other cases, chronic hyponatremia is probable. It is concluded that acute hyponatremia should be treated without delay and rapidly at a rate of at least 1 mmol/L/hour, to prevent severe neurologic damage or death. With respect to chronic hyponatremia, it appeared that severe neurologic complications almost exclusively occurred in patients who were treated with hypertonic or isotonic saline without the addition of furosemide or an osmotic diuretic agent, resulting in a (rapid) correction rate of 0.5 mmol/L/hour or more. In contrast, patients with severe chronic hyponatremia treated with furosemide and isotonic or hypertonic saline almost uniformly did well after rapid correction. Uneventful recovery is also the rule when severe chronic hyponatremia is corrected slowly, at a rate less than 0.5 mmol/L/hour. On pathophysiologic grounds, and bearing in mind that slow correction was used in the majority of reported patients in the literature with severe chronic hyponatremia who recovered without neurologic complications, this treatment modality is preferable. Whenever the available data do not permit a differentiation between acute or chronic hyponatremia, rapid correction has to be pursued by means of administration of hypertonic or isotonic saline together with furosemide [Lasix, a diuretic].”
SUMMARY
When the humidity and heat exceed 60 percent and 60 degrees, athletes are advised to maintain fluid intake between 16-24 ounces per hour [16 for smaller athletes, 24 ounces for larger athletes]. Electrolyte intake with low sodium ENDUROLYTES are accommodated by a rate of 3-6 Endurolytes taken each hour or 1 Endurolyte for each 8 ounces fluid ingested in most subjects in most events, though there are exceptions. Each athlete prone to heat stress should spend time in training for not only fitness but also for physical acclimatization to the conditions forecast on race day. The more fit and the more acclimatized athletes prepare themselves for hyperthermic conditions, the more likely they are to realize intended goal finish times. The average size endurance athlete progresses well on the electrolyte ingredients formulated in Endurolytes taking between 3-6 capsules each hour during aerobic exercise. There are exceptions to this dose rule; a few perform well on only one Endurolyte per hour, while even fewer require more than 6 each hour. One point to emphasize is that as each reference author implies, overdose and underdose repletion rate is not as desirable as adequate repletion in time and dose fashion. It is our contention that low dose repletion rate generates electrolyte balance [homeostasis] without interfering with the electrolyte levels delicately monitored by natural endogenous processes. Taking too much sodium may resolve sodium deficiency temporarily but potentially risks inducing increased distal extremity fluid storage and elevated blood pressure. In addition, taking excessive sodium tends to increase the rate of sodium excretion and in prolonged events may inhibit performance. Taking above 600 mg sodium per hour may be justified in large, overweight, unfit subjects who otherwise deplete sodium stores at a too rapid rate. Excessive water weight gain, increased blood pressure is shown to accompany excess sodium salts dose. The endurance athlete should set out to determine not how to replace all of the sodium lost at once, but how to replace the minimum amount which for most athletes is between 300-600 milligrams per hour. The adjunct to electrolyte balance needs be considered beyond sodium, since other electrolytes contribute to serum minerals and pH balance. The ENDUROLYTE is the model formula suggested for serum mineral and pH balance during prolonged endurance exercise.
REFERENCES
[1] FROM: CARDIOPULMONARY PHYSIOLOGY, Chapter 7 – Renal Considerations,
by Dr. Larry Reinking, Millersville University.
[2] UCLA Endocrinology by Dr. Mark Goodarzi, M.D., SYNDROME OF INAPPROPRIATE ADH
NORMAL PHYSIOLOGY Section @: http://www.endocrinology.med.ucla.edu/siadh.htm
[3] Electrolytes Course Online – N205; Indiana State University, School of Nursing
Mary Bennett, Assistant Professor of Nursing @:
http://www.indstate.edu/nurs/mary/lytenote.htm
[4] American College of Sports Medicine. Position stand on exercise and fluid replacement. Medicine and Science in Sports and Exercise, 28: i-vii, 1996.
[5] Hargreaves M (ed). Fluid and energy replacement for physical activity. Australian Journal of Nutrition and Dietetics. 53 (4:suppl): S2-S48, 1996.
[6] Noakes TD, Norman RJ, Buck RH, Godlonton J, Stevenson K, Pittaway D; The incidence of hyponatremia during prolonged ultraendurance exercise, Med Sci Sports Exerc 1990 Apr 22:2 165-70.
[7] Noakes TD, THE LORE OF RUNNING, Leisure Press, Champaign, Ill., 1991:115-119.
[8] Verde, T, Shephard, RJ, Corey P, Moore R., Sweat Composition in Exercise and Heat, Journal of applied Physiology, 1982;53;6:1541-1543.
[9] Speedy DB, Faris JG, Hamlin M, Gallagher PG, Campbell RG Hyponatremia and weight changes in an ultradistance triathlon. Clin J Sport Med 1997 Jul 7:3 180-4.
[10] Toole ML, Douglas PS, Laird RH, Hiller DB, Fluid and electrolyte status in athletes receiving medical care at an ultradistance triathlon, Clin J Sport Med 1995 5:2 116-22.
[11] Cluitmans FH, Meinders AE; Management of severe hyponatremia: rapid or slow correction? Am J Med 1990 Feb 88:2 161-6.
DISCLOSURE: Bill Misner Ph.D. is the Director of Research & Product Development for HAMMER NUTRITION LTD. Misner has competed in several 50-mile and 24-hour ultramarathon events and is a past multiple National Masters Champion. He was the first 10,000 mile and 20,000 kilometer finisher in the Internet “Million Mile Ultra.” This statement declares competing interests for the low sodium electrolyte formula, “Endurolytes,” marketed by HAMMER NUTRITION LTD.